This is an online e-log book to discuss our patient de-identified health data shared after taking his / her / guardian's signed informed consent. Here we discuss our individual patients' problems through a series of inputs from the available global online community of experts with an aim to solve those patients' clinical problems with collective current best evidence-based information.
This E blog also reflects my patient -centered online learning portfolio and your valuable input in the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and coming up with diagnosis and treatment plans. is an online e-log book to discuss our patient's de-identified health data shared after taking his / her / guardians' signed informed consent. Here we discuss our individual patients' problems through a series of inputs from the available global online community of experts with an aim to solve those patients' clinical problems with collective current best evidence-based information.
CHIEF COMPLAINTS
A 25 year old female came with complaints of headache since 4 days. Nausea and vomiting since 2 days. Fever since 2 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 4days back then She developed severe diffuse headache 4days back which is sudden in onset and progressive in nature and diffuse ,non radiating not associated with photophobia and phonophobia .no aggrevating and relieving factors.
She developed fever 2 days back which is low grade, intermittent, not associated with chills and rigor
She also developed Nausea and vomiting since 2days 3 episodes of vomiting which is non projectile in nature food particles as content and aggravated after intake of food and relieved with medication No h/o blood in vomitings.
No h/o burning micturition, shortness of breath, orthopnea.
No h/o pain abdomen and tenderness.
PAST HISTORY:
N/K/C/O DM,HTN,TB,Asthma, Epilepsy.
H/O Tubectomy done 5yrs ago.
No H/O any blood transfusions done.
FAMILY HISTORY:
Not significant.
PERSONAL HISTORY:
Diet:Mixed
Appetite: decreased
Sleep: adequate
Bowel and bladder movements:regular
No addictions.
GENERAL EXAMINATION:
Patient is conscious, coherent,cooperative, well oriented to time ,place and person.
Moderately built and moderately nourished.
No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy and pedal edema.
VITALS
TEMP:Afebrile
BP:110/80mmHg
PR:80bpm
RR:15cpm
SYSTEMIC EXAMINATION
CVS:S1,S2 heard, no murmurs
•CNS:no focal neural deficit
•RS:Trachea central, bilateral air entry present, normal vesicular breath sounds heard.
•Per abdomen examination:soft, non tender,no guarding and no rigidity and no organomegaly and bowel sounds are heard.
PROVISIONAL DIAGNOSIS:
HEADACHE UNDER EVALUATION.
INVESTIGATIONS:
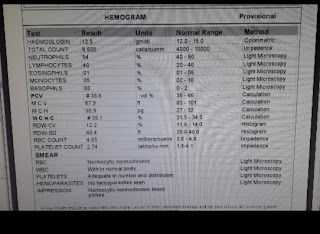
HEMOGRAM:
Hb:12.5gm/dl(13-17)
Total count:8,500cells/cumm(4000-10000)
Neutrophils:54%(40-80)
Lymphocytes:40%(20-40)
Eosinophils:1%(1-6)
Monocytes:5%(2-10)
PCV:35.6 vol%(40-50)
MCV:87.9fl(83-101)
MCH:30.9pg(27-32)
MCHC:35.1%(31.5-34.5)
RBC:4.05millions/cumm(4.5-5.5)
PLATELETS:2.74lakhs/cumm(1.5-4.1)
COMPLETE URINE EXAMINATION:
Albumin:nil
Sugars:nil
Bile salts:nil
Bile pigments:nil
Pus cells:2-3
RANDOM BLOOD SUGAR
94mg/dl(100-160)
LIVER FUNCTION TESTS
Total bilirubin:1.02mg/dl(0-1)
Direct bilirubin:0.19mg/dl(0.0-0.2)
AST:33 IU/L(0-35)
ALT:29 IU/L(0-45)
ALP:252 IU/L(56-119)
Total protein:7.5gm/dl(6.4-8.3)
Albumin:3.75gm/dl(3.2-4.6)
Albumin/globulin ratio:1.00.
RENAL FUNCTION TESTS:
S.UREA:21mg/dl(17-50)
S.CREATININE:0.6mg/dl(0.8-1.3)
S.URIC ACID:3
CALCIUM:10.4mmol/l
PHOSPHATE:3.9
SODIUM:135mEq/L(135-145)
POTASSIUM:4.4mEq/L(3.5-5.1)
CL:102mEq/L(98-107)
SEROLOGY
HbsAg:negative
HIV: negative
HCV:negative
USG
Multiple. Calculi noted in gall bladder of size 13 to 14 mm
ECG
DIAGNOSIS:
Headache under evaluation
With Cholelithiasis.
TREATMENT:
1.TAB.NAPROXEN 250mg PO/BD
2.TAB.PAN 40mg PO/OD
3.TAB.ZOFER 4mg PO/BD
4.MONITER VITALS FOR EVERY 4TH HOURLY






Comments
Post a Comment